Cerebral palsy. Are you familiar with the term? CP is a motor anomaly which results from injury to motor centers of the brain. The damage occurs before, during, or after birth, and is usually non-progressing. The severity of the motor impairment differ greatly between individuals, according to where the damage lies. Damage to the motor centers of the brain may occur concurrently with other parts as well, which may result in mental retardation, perceptual deficits, sensory problems, and/or behavioral disturbances. The severity of CP patients may vary from mild to severe. CP may be divided depending on time of onset, neuro-muscular characteristics or parts of body affected. This will not be discussed in detail here, but may be read further in other articles such as this one.
So... how did I find a CP patient?
on 26th July, a guy walked into our optical shop at around 8 p.m, along with his mother, and an invalid in a wheelchair, pushed in by an assistant. He searches for my boss, who's out for some errands. Apparently, the invalid is his brother, who requires a routine eye examination. Well... as my boss is out, it is my duty to carry out the eye examination. I had to admit, I was nervous. Especially when his brother whispers to me that the invalid has cerebral palsy.
This is not my first time dealing with people with cerebral palsy. I had previously encountered another case in UKM clinic. However, it is different this time, as I was on my own. With no friends or supervisors to help me out, only the brother. I took a deep breath, and attempted it anyway.
So... what should I do? Hm... of course, first of, as in anyone else's visit, I attempted to take down his VA (visual acuity with the Snellen Chart). I was lucky that he did know his alphabets, but halfway through, maybe due to fatigue, or that he cannot see the letters any more. I couldn't verify which is which, as he responds an 'S' to all letters I showed him afterwards. After a few more tries, I stopped taking the acuity, and did an over-refraction with him wearing his glasses. This is done simply using my retinoscope. Thankfully, his current refractive error did not change much with his glasses, hence I did not prescribe any new lenses. I attempted ophthalmoscopy, whereby I manage to view some of the fundus (the retina- where light is received by our eyes to be transmitted to the brain), but not the cup and disc as the eyes are not fixating well (especially the left eye). Under the slit lamp, no abnormality was found.
For this visit, the patient was not given any new pairs of glasses. His current one is still good for distance, and he had made another previously for reading [the patient is in his 60s]. His brother reported that he has been seen wearing his reading pair for daily use and vice versa at his care-center often. Hence, to make it easier for his carers to identify and differentiate the two, I marked the current one with tape.
-----
Well... so that is how I handled the patient at the time. However at the back of my mind, i kept wondering on what visual problems people with cerebral palsies usually have, and how should we really manage them? Hence, I did some reading and research. I found many interesting facts regarding vision conditions of people with cerebral palsy and the ways to manage them.
First and foremost, the biggest question that looms over my head when the patient arrived (other than how well will he be able to respond to my questions) is regarding the visual problems that the CP patients might face. Identifying their common visual problem makes it easier to focus one's examination and assist in any particular problem they might face. According to the Ettinger, who complied numerous studies regarding CP, the most common problems for a CP patient are strabismus (30-60%), amblyopia (, significant refractive errors, accommodative deficits (100% accommodative insufficiency) and visual perceptual problems (78%). Nystagmus and optic atrophy have also been reported, but less frequently (18-19% and 4-10% respectively).
Strabismus [picture courtesy of Google search]
Now that we had identified some of the problems the patients commonly face, we should examine the patients best as we can. The first thing to do is, of course, to take a detailed history, in order to identify the extension and type of CP, the medical practitioners involved, past operations and treatments, education, etc. During this time, one should attempt to gain the patient's trust, as well as the trust of the person who cares for him. Next is to attempt to take the visual acuity as best as we can. There is a limitation in the accuracy, as the patient may not be able to communicate that well, and often have reduced mental capacity. Some tools that may help are Tumbling E chart, Forced Preferencial Looking, and optokinetic nystagmus (OKN). A precise and reliable, yet seldom available visual acuity test is the sweep-VEP.

Various test charts [picture courtesy of google search]
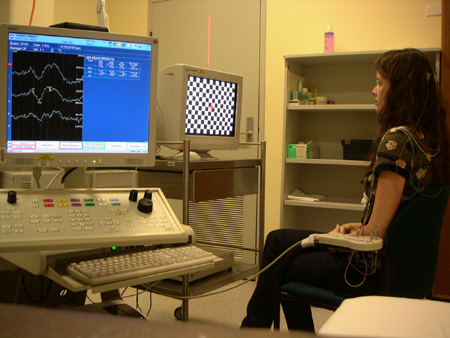
VEPs [picture courtesy of google search]
Oculomotor assesment may be made using bright, attractive target via cover test, Hirschberg test, pursuit, saccades and near point of convergence. Refractive status may be determined by refraction and keratometry reading, when possible. The use of subjective refraction depends on the patient's ability to respond and participate. Accommodation status may be tested by testing monocular estimation method via dynamic retinoscopy. Ocular health testing is also very important, hence direct or indirect ophthalmolscope is important. If possible, dialation of the pupil may be used.
The next question that pops up, after the examination, is how to treat these conditions on a CP patient? Will treatment help improve their vision? According to Ettinger, there are four different aspects in addressing this issue, which are:
- Communication with caregiver, parents and other medical professionals;
- Binocular dysfunctions impact to the patient, whether it reduces the patient's functionality or not, especially in doing prolonged near work such as rading and writing. There are vision therapies which the patient may undergo in order to improve their binocular vision condition. Articles regarding the types of vision therapy available may be found in the bottom of this article.
- When to prescribe glasses, some suggest that refractive error of myopia, hyperopia or astigmatism of 1.50D or more should be prescribed (Ettinger, 1991), whether the condition is symptomatic or asymptomatic. Taub (2006) suggests that myopia more than 8.00D, hyperopia and astigmatism more than 4.00D should be corrected.
- Decision regarding strabismus surgery. As the strabismus incident is very high in this population, parents would likely discuss the option of surgical intervention with optometrist, who needs to weight out the option carefully, regarding the risk posed by the vulnerable population, neurological basis of the strabismus, and the guarded success rate of strabismus surgery among CP patients.
In a nutshell, optometrist play an important role in ensuring visual functioning of patients with CP. Optometrist need to realize that this population must obtain proper eye care in order to ensure that they may function better and not be limited by visual capabilities.
Resources:
http://www.optometry.co.uk/uploads/articles/c6292bb74eab99ac77dac5d0f67594c4_Taub-10206.pdf
http://www.oepf.org/jbo/journals/2-5%20ettinger.pdf
http://www.oepf.org/ICBOFlash/Posters/Scheulke.pdf
http://www.drjoelwarshowsky.com/Principles_of_Optometric_Rehabilitation.pdf
http://www.nature.com/eye/journal/v9/n1/pdf/eye199523a.pdf

No comments:
Post a Comment
Comments, discussions, and questions are welcome!